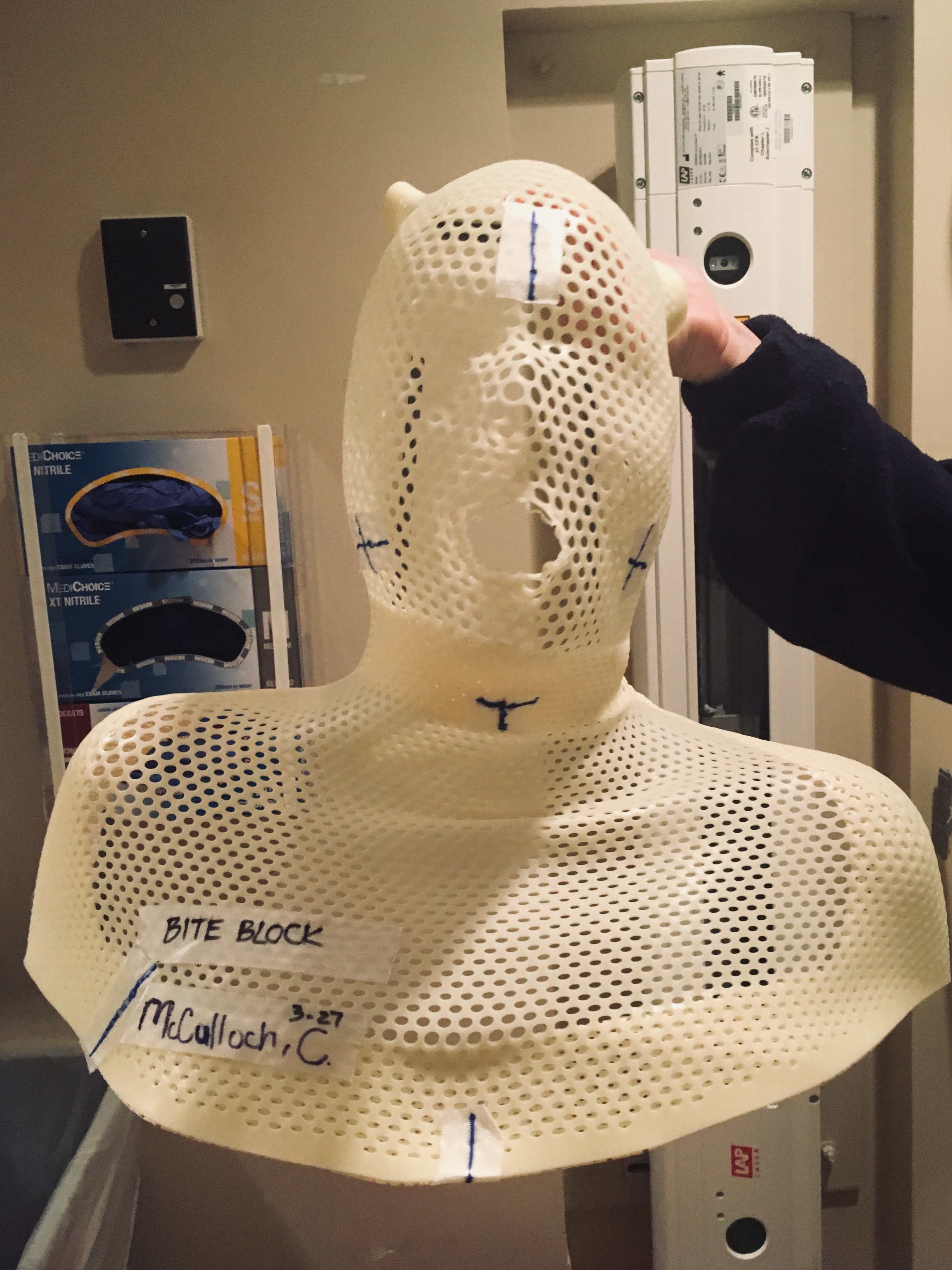
I haven’t written in a while because I’ve been waiting for “news” to report. That is to say, some kind of change or improvement. There has been change and, I suppose, modest improvement. The sores on my tongue and the walls of my mouth have more or less healed, and the pain I felt in my throat when I swallowed has migrated to my right ear. In fact, that’s pretty much the only pain I feel anymore and it’s lessening, little by little, each day. This is most fortunate, considering the fact that I’ve been weaning off of Oxycodone over the past week. Next week, I will be weaning off of Gabapentin, but supplementing all the while with Advil and Tylenol. I also feel my energy returning, but slowly and in small increments. A single outing or errand will still wear me out more than it ever used to.
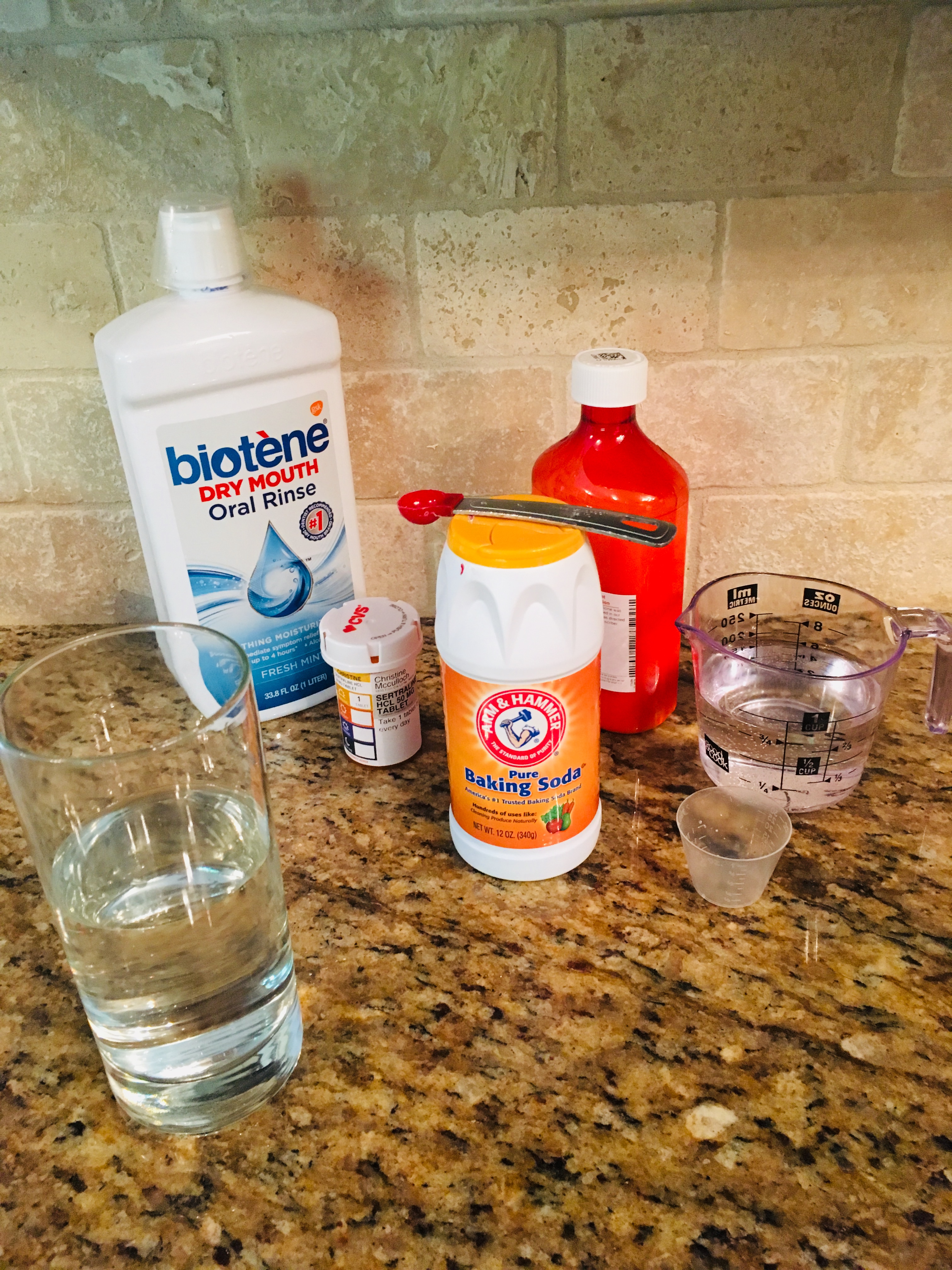
I think the next challenge in my healing process will probably be figuring out food. My last actual meal was on April 14, which I know thanks to this blog. I’ve been on a liquid diet for forty-four days now, and a limited one, at that. Given the changes to my taste buds, the only things I’ve found tolerable over the past month-and-a-half have been water, Ensure, butternut squash soup, drinkable yogurt, and vanilla milkshakes. That’s it. That’s what I have every. single. day. At the behest of my speech therapist, I will try a bite of something else here and there (applesauce, mashed potatoes, cottage cheese, other soups, etc.), but these either taste terrible, or I can’t manage to swallow them. My natural saliva production, which I’ve learned helps break down food as you chew, has gone completely haywire, and food will simply get stuck to my teeth, tongue, or the roof of my mouth, causing pain and discomfort. It’s really very frustrating. So, I stick with what I know works because my body needs calories to heal.
Much like a recovering alcoholic, I’ve started to realize how heavily our social rituals revolve around food and drink. It’s hard when you can’t participate, and a little lonely. But it’s not the end of the world. And, in my case, it’s hopefully temporary. I just wish I knew when I’ll be able to eat again. No one has told me, and I can’t find it in the two other MASC blogs I’ve located on the internet. It’s hard to continue to be patient, and to live with uncertainty. That’s pretty much the crux of this entire ordeal, in fact, from my diagnosis right up until now. A serious illness pulls the rug of certainty out from under you, and it’s difficult to regain your footing. I still have my sea legs, I guess, and might for a while.